Testing for inherited thrombophilias following venous and arterial thrombotic events remains controversial. These conditions are associated with an increased risk of initial and recurrent venous thromboembolism (VTE) and, in some cases, arterial events such as strokes and myocardial infarctions. However, testing for them in unselected patients with thrombotic events is not associated with lower recurrence rates, and other risk factors may be more clinically useful for determining whether and for how long to anticoagulate. Further, these tests are expensive and in the setting of an acute thrombosis, many may result in false positives. As such, the American Society of Hematology and American Society for Clinical Pathology recommended in their Choosing Wisely campaigns to not test for inherited thrombophilias after a provoked VTE or in the acute setting, respectively. The AHA/ASA determined that the utility of thrombophilia screening in stroke patients was unknown in its 2014 guidelines.
This single institution, retrospective study reviewed all instances of inpatient inherited thrombophilia testing in 2019 at Thomas Jefferson University Hospitals, including its 3 primary hospitals in Philadelphia, PA. Tests included those to evaluate the following conditions: Factor V Leiden (FVL); prothrombin G20210A mutation; Protein C, S, and antithrombin deficiency; hyperhomocysteinemia; and plasminogen activator inhibitor-1 (PAI-1) elevation. The study included 231 patients, among whom a total of 872 tests were sent. Tests sent for non-thrombotic indications, such as homocysteine for B12 or folate deficiency, or in patients with a known deficiency were excluded.
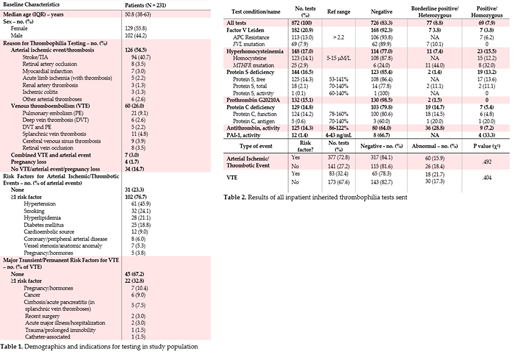
Median age of the patients was 50.8 years (IQR 38-63) and 129 (55.8%) were female. Diagnoses for which testing was sent and predisposing risk factors are summarized in Table 1. Arterial events were most common (54.5%), followed by VTE (26.0%). 14.7% of patients had no documented thrombosis, ischemic event, or pregnancy complication. Arterial events primarily included stroke/TIA (74.6%), and 76.7% of patients had at least one documented risk factor for these conditions. VTE was associated with a major transient risk factor or cancer in 32.8% of patients.
Among all inherited thrombophilia tests sent, the most common were for the evaluation of FVL (20.9%), hyperhomocysteinemia (17.0%), Protein S deficiency (16.5%), prothrombin G20210A mutation (15.1%), Protein C deficiency (14.8%), and antithrombin deficiency (14.3%) (Table 2). Overall, 83.3% of tests were normal. Tests that were most frequently abnormal included MTHFR mutation (76.0%), antithrombin (36.0%), Protein C antigen (40.0%), PAI-1 (33.3%), and total Protein S (22.2%). Given our lab's references ranges, values for antithrombin, and Protein C antigen and function, and total Protein S that fell below normal but >60% were deemed "borderline positive." The likelihood of an abnormal result was not significantly different in cases of unprovoked VTE or arterial event without a risk factor, compared to those with risk factors. All charts were reviewed, including both inpatient and outpatient notes, to determine short- and long-term clinical decision-making. Importantly, among all positive tests, clinical management was not definitively changed in response to the test result in a single case. In two patients, it was unclear whether anticoagulation was continued based upon the test result. Both patients had heterozygous FVL mutations. Most positive results were deemed by the treating clinicians to be due to the acute thrombotic episode. Last, the hospital's chargemaster was queried, showing that these tests were associated with $398,912 in total charges.
This single-institution retrospective study of inpatient inherited thrombophilia tests reveals the limited benefit of thrombophilia testing in the acute setting. Arterial ischemic/thrombotic events were the most common indication for testing, yet over 3/4 of patients had at least one risk factor. Nearly a third of patients with VTE had a major provoking factor, patients in whom thrombophilia testing is not recommended. While nearly 17% of tests returned abnormal, not one was associated with a clear change in clinical management. Despite limited clinical utility, costs of these tests are high. These data justify education and pathway implementation aimed at decreasing inpatient utilization of thrombophilia tests.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal